
The aim of this study was to investigate whether this artifact was related to the presence of radiologic alveolar-interstitial syndrome in a series of critically ill patients. Clinical experience suggests that the comet-tail artifact arising from the lung-wall interface is very often seen in patients suffering from acute pulmonary edema. Likewise, the horizontal artifact arising from the lung surface and its potentially normal significance have not been described. To our knowledge, the normal or pathologic nature of the comet-tail artifact at the lung surface has not been established. The artifact described in the present study corresponds to a long variety of comet-tail artifact, the one that extends to the edge of the screen. Besides, in the first study ( 9), long and short varieties of comet-tail artifacts are presented without distinction. As a consequence, no practical use had been made from this artifact at the lung level. It had also been noted at the lung surface in normal or pathologic conditions ( 9, 11), although no correlation had been made with a pathologic feature. The comet-tail artifact was described in 1982 concerning an intra-hepatic shotgun pellet ( 9). According to a review of the literature, narrow repetition artifacts are known as “comet-tail” ( 9) or “ring-down” ( 10) artifacts. The other is a roughly vertical narrow-based artifact spreading up to the edge of the screen. One type is a roughly horizontal repetition artifact. In fact, two opposed types of artifacts can clearly be differentiated arising from the lung surface. On the other hand, ultrasound patterns of the aerated lung are not well known, and airy artifacts arising from the lung surface have not been extensively studied. Yet clinical experience and review of the literature show that lung ultrasound has been previously proposed for diagnosing pneumothorax ( 1-4) or alveolar consolidation ( 5-8). The lung is therefore usually considered poorly accessible to ultrasound. Can ultrasound, a noninvasive, easily implemented technique, be of any use? Basically, the problem is that air stops the progression of the ultrasound beam, and only reverberation artifacts are visible under the lung surface. However, in critical care units, chest X-ray is performed at the bedside and technologic deficiencies may make this diagnosis difficult. The diagnosis of alveolar-interstitial syndrome is based on chest X-ray. In conclusion, presence of the comet-tail artifact allowed diagnosis of alveolar-interstitial syndrome.
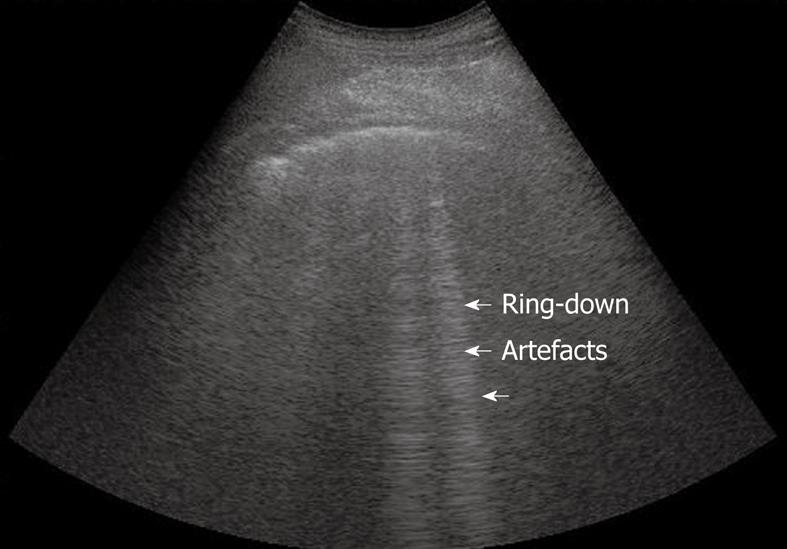
Tomodensitometric correlations showed that the thickened sub-pleural interlobular septa, as well as ground-glass areas, two lesions present in acute pulmonary edema, were associated with the presence of the comet-tail artifact. It was absent or confined to the last lateral intercostal space in 120 of 129 patients with normal chest X-ray (specificity of 93.0%). This pattern was present all over the lung surface in 86 of 92 patients with diffuse alveolar-interstitial syndrome (sensitivity of 93.4%).

The ultrasonic feature of multiple comet-tail artifacts fanning out from the lung surface was investigated. The antero-lateral chest wall was examined using ultrasound. Can ultrasound be of any help in the diagnosis of alveolar-interstitial syndrome? In a prospective study, we examined 250 consecutive patients in a medical intensive care unit: 121 patients with radiologic alveolar-interstitial syndrome (disseminated to the whole lung, n = 92 localized, n = 29) and 129 patients without radiologic evidence of alveolar-interstitial syndrome.


 0 kommentar(er)
0 kommentar(er)
